40YR OLD MALE WITH CKD
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
CHIEF COMPLAINTS
PT IS BROUGHT TO CASUALITY WITH
C/O PAIN ABDOMEN SINCE 2 DAYS
VOMITING SINCE 1 DAY
DECREASED URINE OUTPUT SINCE 1 DAY
NO URINE OUTPUT SINCE 8 HOURS
HOPI-
PT WAS APPARANTLY ASSYMPTOMATIC 3 DAYS BACK THEN HE DEVELOPED PAIN ABDOMEN ; DRAGGUNG TYPE OF PAIN IN EPIGASTRIUM AND UMBILICAL REGION NOT RADIATING INCREASE WITH FOOD INTAKE
DISTENTION OF ABDOMEN IS PRESENT
VOMITINGS PRESENT 1 EPISODE PER DAY
NOT BILIOUS AND NON PROJECTILE
NOT BLOOD TINGED
DECREASED URINE OUTPUT SINCE 1 DAY
NO FACIAL PUFFINESS,FEVER,BURNING MITURITION.
NO H/o SOB, CHEST PAIN,BLURRING OF VISION,HEADACHE.
PAST HISTORY
HE HAD NEUROGENIC BLADDER AT AGE OF 7 YEARS
HE HAD A SWELLING IN MIDLINE LOWER LUMBAR REGION WHICH IS ABOUT 2×2 CM SINCE BIRTH
AT THE AGE OF 7 YEARS HE GOT OPERATED ON THAT SWELLING AND SINCE THEN HE DEVELOPED NEUROGENIC BLADDER FOR WHICH HE WAS CONSERVATIVELY MANAGED WITH FEW MEDICATION
K/C/O CKD SINCE 10 YEARS ON CONSERVATIVE MANAGEMENT AND ON FOLEYS
K/C/O HTN SINCE 1 YEAR IT IS DIAGNOSED ON A ROUTINE EXAMINATION AS A PART OF TREATMENT TO CKD
N/K/C/O DM; ASTHMA; CAD; THYROID ; EPILEPSY
PERSONAL HISTORY
MIXED DIET
APPETITE- DECREASED SINCE 1 WEEK
BOWEL- REGULAR
BLADDER NEUROGENIC
ADDICTIONS-
SINCE 20 YEARS OCCASIONALLY
STOPPED SINCE 4 DAYS
FAMILY HISTORY
NOT SIGNIFICANT
GENERAL PHYSICAL EXAMINATION-
PT IS CONSCIOUS COHERENT COOPERATIVE
MODERATELY BUILT AND NOURISHED
NO SIGNS OF PALLOR ICTERUS CYANOSIS CLUBBING GENERALISED LYMPHADENOPATHY PEDAL EDEMA
VITALS
TEMP- 99F
BP-140/90 mm of Hg
PR- 105bpm
RR-28 cpm
Spo2- 99%
Grbs-108 mg%
SYSTEMIC EXAMINATION
CVS-S1; S2 HEARD, NO MURMURS
RS- BAE+ NVBS+
ABDOMEN-
INSPECTION-
SHAPE- DISTENDED
HERNIAL ORIFICES - NORMAL
NO VISIBLE PULSATIONS, NO VISIBLE PERISTALSIS
NO SCARS; NO SINUSES, NO FISTULAS
PALPATION- ALL INSPECTORY FINDINGS ARE CONFIRMED BY PALPATION
NO LOCAL RISE OF TEMPERATURE AND TENDERNESS
NO PALPABLE MASS
NO ORGANOMEGALY
PERCUSSION-
DULL NOTE ON RIGHT LUMBAR; LEFT LUMBAR; RIGHT ILIAC ; LEFT ILIAC REGIONS
ASCULTATION-
BOWEL SOUNDS HEARD
CNS EXAMINATION
LEVEL OF CONSCIOUSNESS - CONSCIOUS
SPEECH - NORMAL
NO NECK STIFFNESS
KERNIGS SIGN- ABSENT
CRANIAL NERVES- NORMAL
MOTOR SYSTEM- RT
LT
TONE UL N N
LL N N
SENSORY SYTEM - NORMAL
GLASGOW SCALE- EVM 15/15
POWER RT LT
UL 3/5 3/5
LL 3/5 3/5
REFLEXES RT LT
BICEPS +3. +3
TRICEPS. +3. +3
KNEE REFLEX +3. +3
CEREBELLAR SIGNS- COULNOT BE ELEICITED
GAIT - ABNORMAL
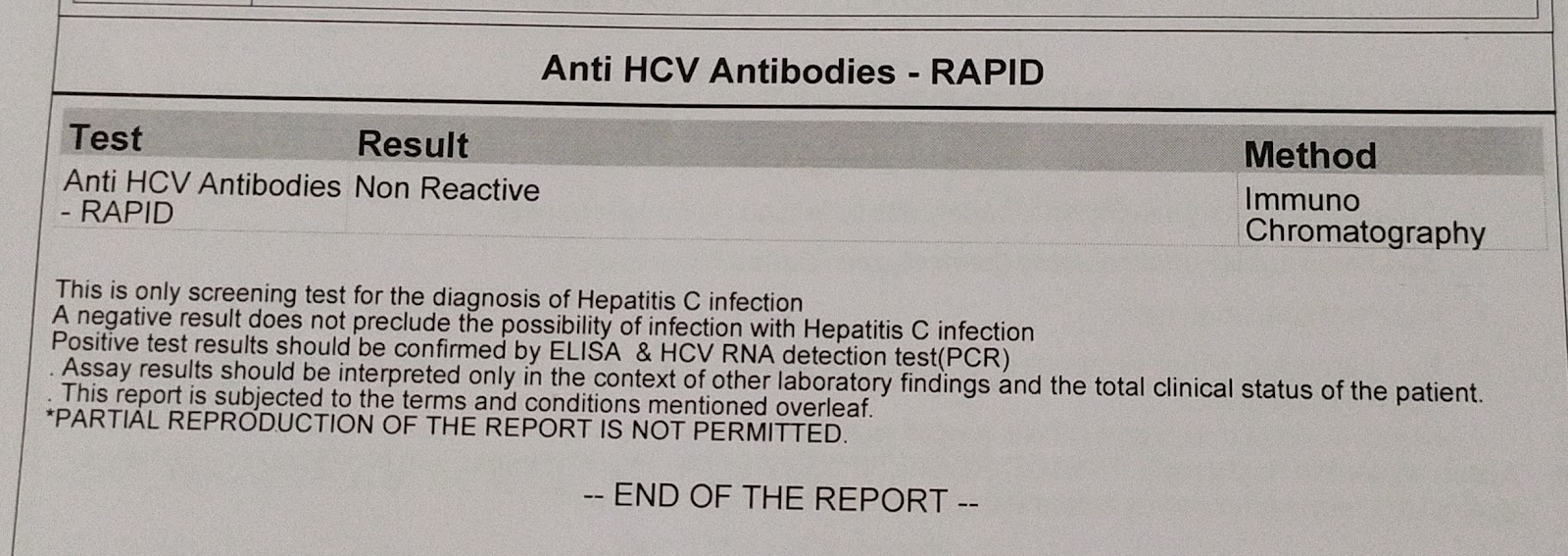
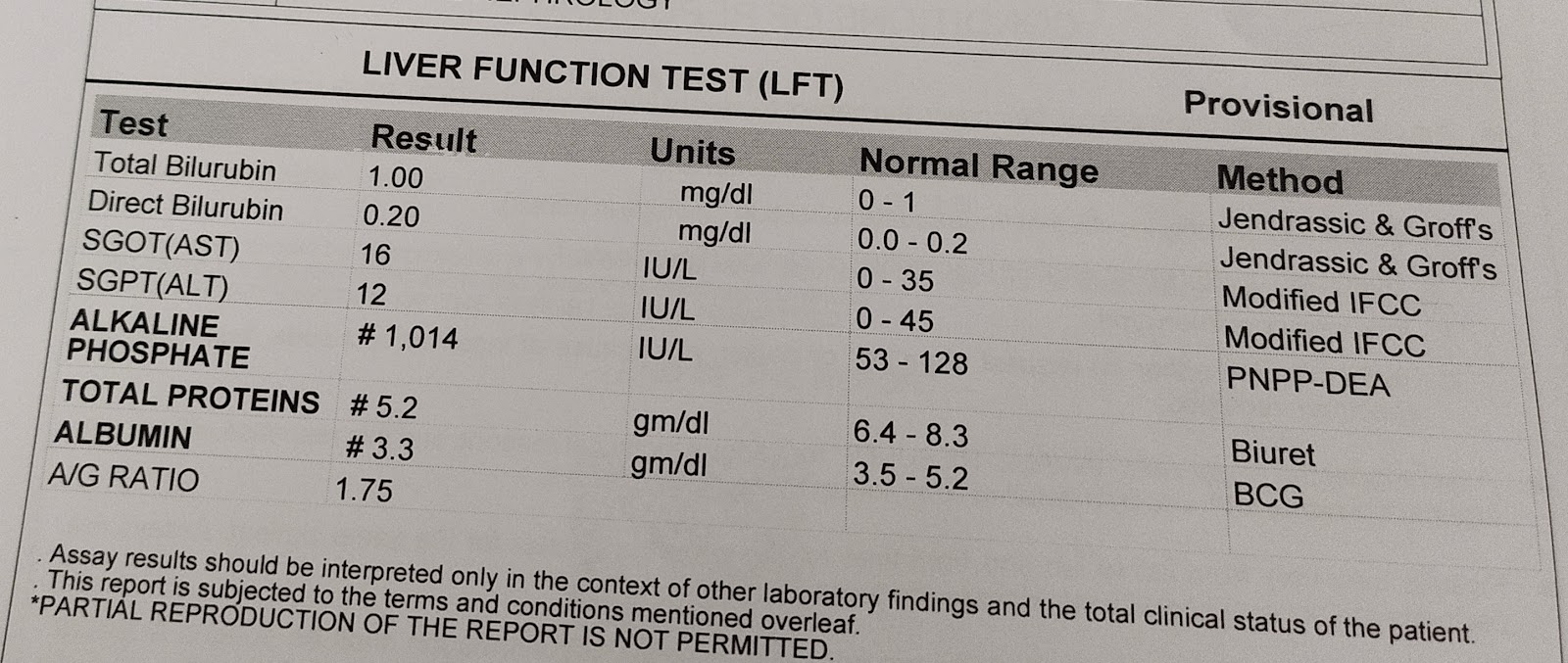
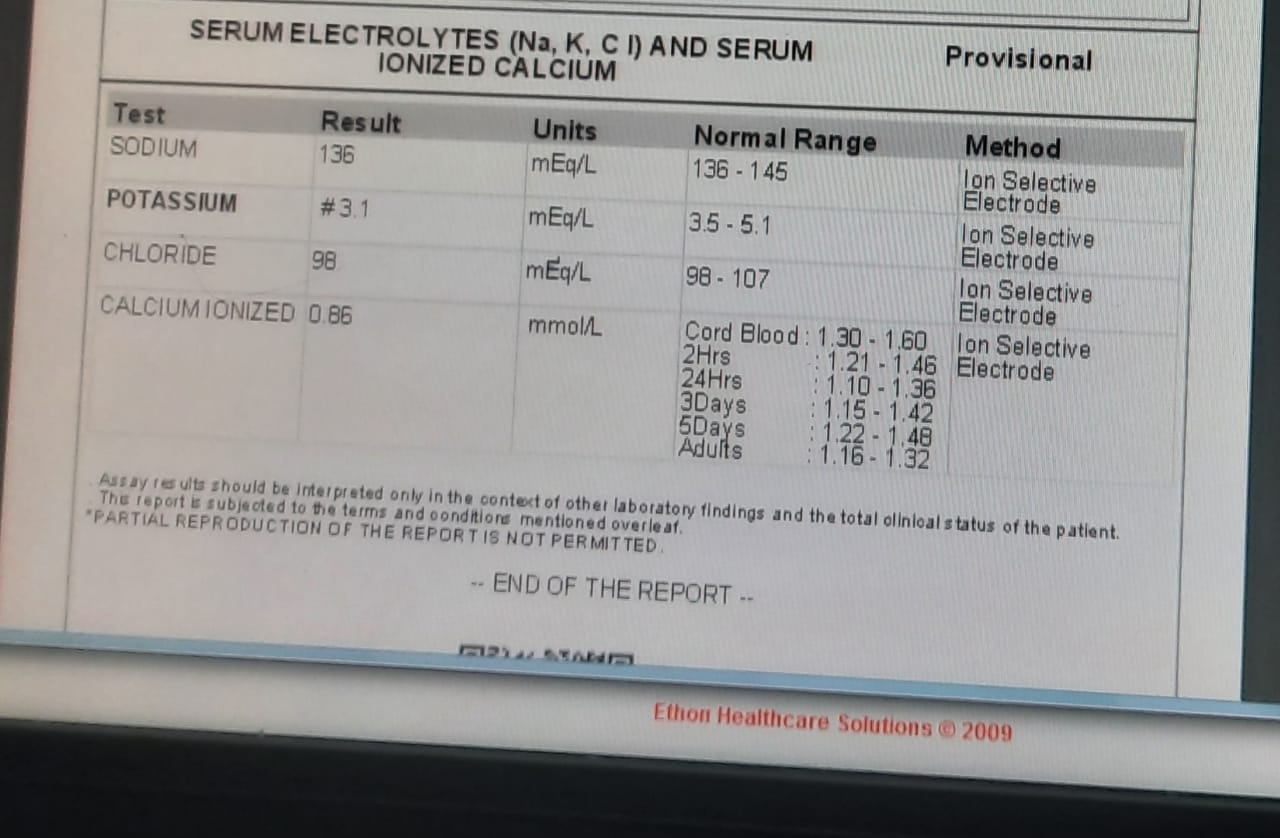
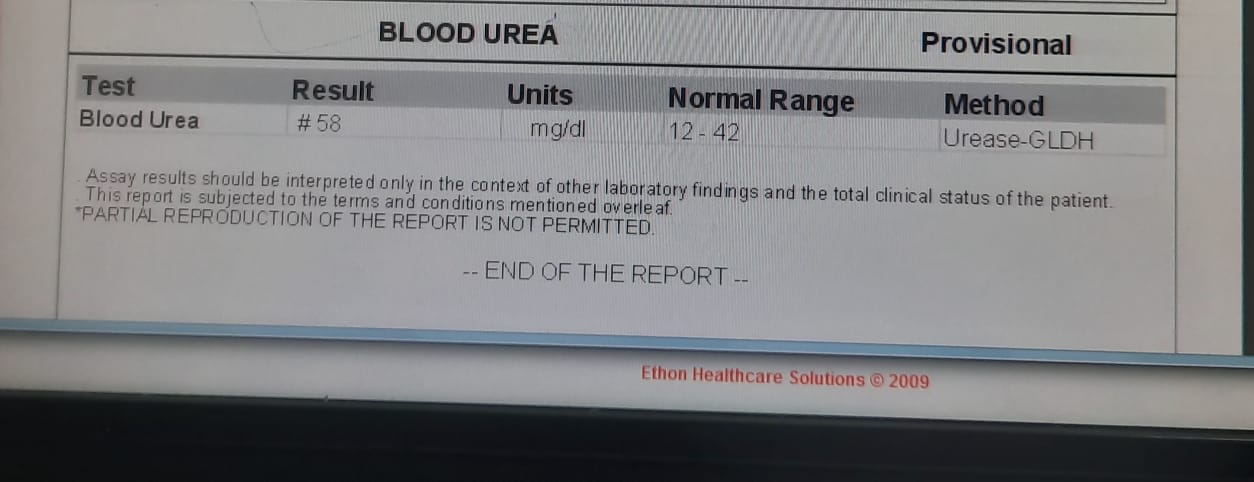
INVESTIGATIONS
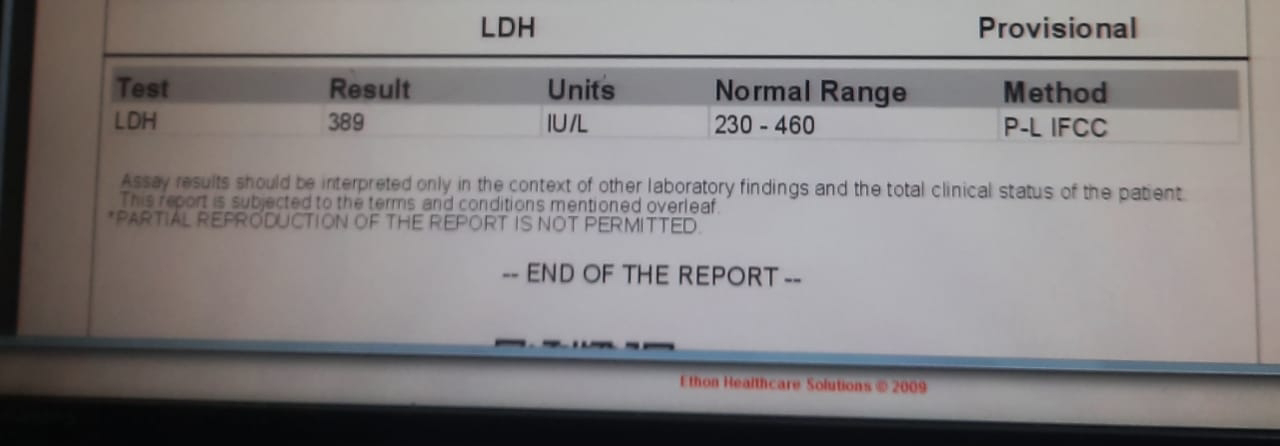
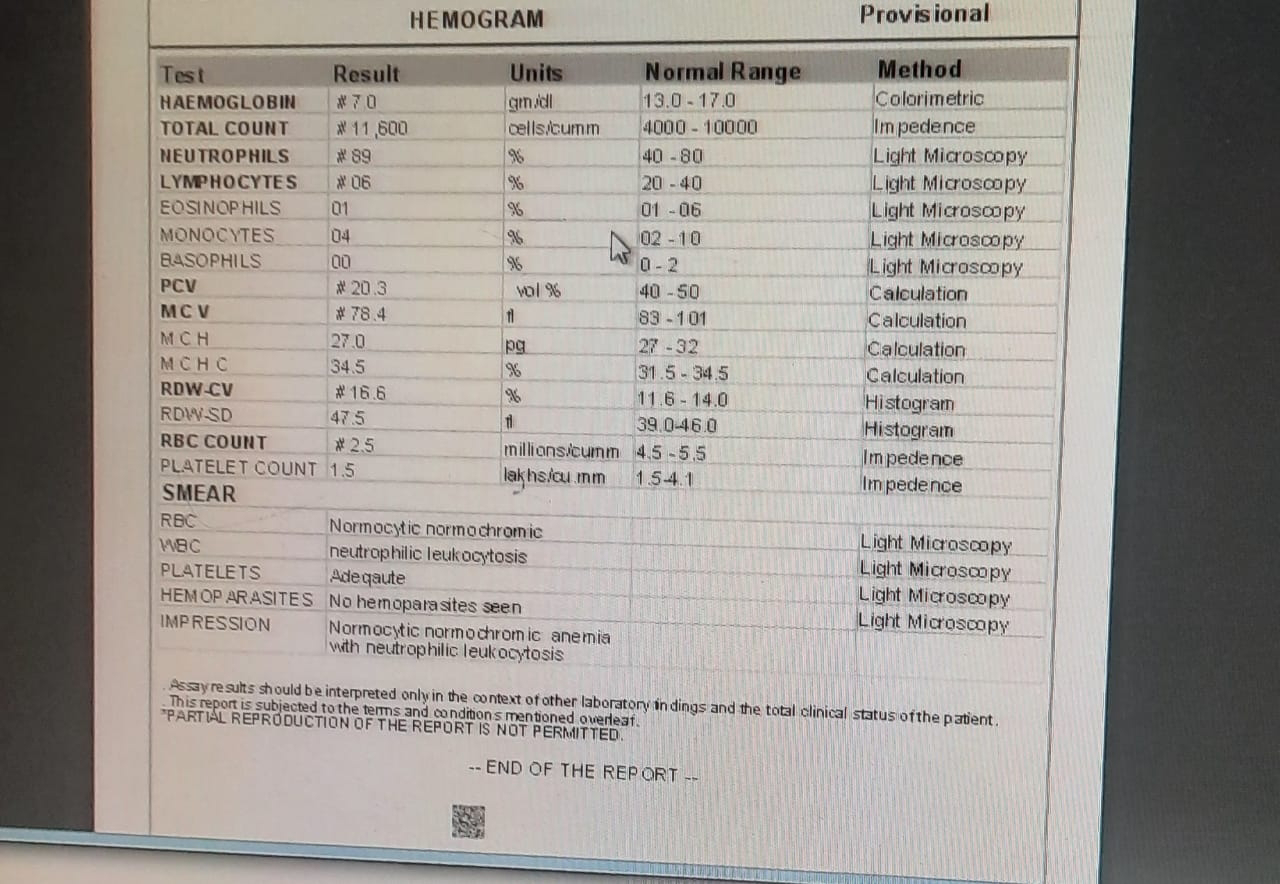
27/10/23
30/10/23
TREATMENT
1.FLUID RESTRICTION LESS THAN
1.5 L/DAY
2.SALT RESTRICTION LESS THAN
2 G /DAY
3.INJ PAN 40 MG IV/OD
4.INJ ZOFER 1G IV /SOS
5.INJ LASIX 40MG IV/BD
6.INJ BUSCOPAN 1 AMP /IM/SOS
7.INJ EPO 4000 IV /SC/ ONCE WEEKLY
8.TAB.NODOSIS 500 MG PO/TID
9.TAB OROFER XT PO/OD
10.TAB.SHELCAL - PO/OD
11.TAB ARKAMINE 0.1MG /PO/TID
12.TAB MINIPRESS XL 2.5 MG PO/OD
13 TAB SEVELEMAR 400MG /PO/BD
14.SYP POTKLOR 10ML IN GLASS OF WATER PO/TID



























Comments
Post a Comment